2018 is the year of running (at least for Dr. Emily). With this, Dr. Emily is spending more time with runners, and she is hearing more about aches and pains with runners. Enter this blog post about IT Band Syndrome!
Definition and Causes of IT Band Syndrome
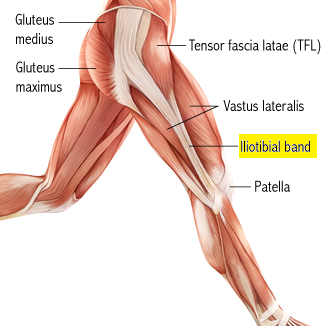
First things first – what is the IT Band? IT stands for iliotibial; the IT band runs from your ilium to your tibia. The ilium is the science term for your hip bone and your tibia is one of the bones in your leg. Check out this picture to better visualize the IT band.
Looking at this photo, you can see the white tendinous fibers if the IT band. The top part of the IT band is thinner and fanned out. It is made up of fibers from tensor fascia latae (TFL) in the front, gluteus maximus in the back, and gluteus medius on the underside. As you travel down the IT band, fibers from vastus lateralis (one of the 4 muscles to make up your quadriceps) contribute a bit. The lowest portion of the IT band is a narrow, thick band that you can feel just above your knee.
So now that we are familiar with the IT band, we can look into IT band pains. IT band pains can come whenever the IT band isn’t able to move and support your body the way it is supposed to. If any of those muscles we talked about get too tight/aggravated, it can pull on the IT band and alter the biomechanics of your hip, knee, and leg. But there’s even a bigger picture than that! The IT band is not only connected to those muscles but to the ilium and the tibia. Both of those bones also serve as attachement sites to MANY other muscles. That means that any number of muscles can affect the ability of the IT band to work as it is supposed to.
There are some activities that can put more stress on the IT band. These include running downhill, running on slanted surfaces, always running on the track in the same direction, or simply over exertion. Wearing shoes that are worn out can also change your biomechanics and put more stress on the IT band.
Signs and Symptoms
IT band pain presents differently depending on where the problem started. Some common symptoms are:
- Nagging pain on the outside of your knee
- Sharp pain at the outside of your knee
- Swelling pain around your knee
- Feeling a click, pop, or snap on the outside of your knee
- Pain up and down the outer part of your upper leg
Many times the pain around the knee comes on during a certain part of a run and gradually gets worse. Many runners will feel that this pain is worse while going downhill.
The pain may also be noticed while cycling. It can come and go during the downward pedal stroke and upward pedal stroke (when your knee is bent around 30 degrees).
Sometimes the pain will go away with rest, but it will return with activity.
Chiropractic Approach
First off, a chiropractic exam is performed to determine the cause of the IT band irritation. A series of orthopedic tests, movement assessments, and palpation of the muscles and joints give us a good understanding of what is causing your pain. Through this exam, we can usually identify what the cause(s) of the pain are. The cause of the IT band syndrome dictates the treatment.
If the cause is any of the muscles whose fibers directly feed into the IT band, the treatment will likely be focused on soft tissue therapy to those muscles. Manual soft tissue treatments (like massage) and instrument assisted soft tissue treatments (see this page for more info) are often very effective in treating IT band syndromes caused by this.
If the cause is due to joint restrictions (either in your feet, ankle, knee, hips, pelvis, or low back), we can correct those through chiropractic adjustments.
If the cause is due to muscle imbalances pulling on the ilium or tibia restricting the natural movements, we will work on correcting that imbalance by strengthening/activating the weakened muscles and stretching the tight/overactive muscles.
Some patients may have multiple causes contributing to their IT band syndrome, so we treat all the causes. We are also a big fan of home stretches and exercises to help eliminate future flair ups. Many patients benefit from foam rolling or using massage sticks over the musculature of their thighs and legs.
After your first treatment, we will go through specfic exercises and stretches that are targeted towards correcting YOUR causes of IT band syndrome.
There is no need to live with insistent, irritating pain. Call us today!